Varicose veins aren’t just a cosmetic nuisance; they can indicate underlying venous disease that, if left untreated, may reduce mobility and quality of life. For those who suspect a problem, seeking varicose vein treatment in Round Rock connects patients with qualified specialists who provide safe, effective care and lasting relief. This guide explains what causes varicose veins, what a vein specialist does, how diagnoses are made, the spectrum of treatment options, and practical tips for choosing a clinic and navigating insurance—designed to help busy professionals make well-informed choices quickly and confidently.
Understanding Varicose Veins: Causes, Symptoms, and When They Matter
Varicose veins are dilated, twisted veins usually visible beneath the skin of the legs. They develop when venous valves, tiny flaps that keep blood flowing toward the heart, become weak or damaged, allowing blood to pool. Common contributing factors include genetics, age, prolonged standing or sitting, pregnancy, obesity, and a history of deep vein thrombosis.
Symptoms range from mild to severe. Many people first notice cosmetic bulging or discoloration. Others experience aching, heaviness, leg fatigue, swelling, itching, and cramping. In advanced cases, skin changes (hyperpigmentation), venous ulcers, or bleeding from superficial veins can occur.
When do varicose veins matter clinically? If symptoms interfere with daily activity, sleep, or work productivity, or if complications like skin changes or ulceration appear, timely evaluation is warranted. For professionals who travel, manage teams, or depend on physical stamina, early treatment can prevent deterioration and preserve quality of life.
Recognizing early signs and consulting a specialist instead of self-treating with only creams or over-the-counter compression can change outcomes. A specialist evaluates both visible veins and the underlying venous system to determine whether treatment is medically necessary and which approach is safest and most effective.
Why a Varicose Vein Specialist Matters: Qualifications and Expertise
A varicose vein specialist typically comes from fields such as vascular surgery, interventional radiology, or phlebology (vein medicine). Key qualifications to look for include board certification in a relevant specialty, specific training in venous procedures, and an established track record of treating a wide range of venous disorders.
Specialists bring several advantages over general practitioners:
- Diagnostic precision: They interpret duplex ultrasounds and other imaging to locate reflux and map the venous system.
- Procedural expertise: They perform minimally invasive procedures, endovenous ablation, sclerotherapy, and VenaSeal with low complication rates.
- Tailored care: They design staged treatment plans for complex cases, combining therapies when needed and focusing on long-term outcomes rather than quick fixes.
Experience matters; clinicians who treat higher volumes of venous disease tend to have better outcomes and fewer repeat procedures. Peer-reviewed publications, patient outcome data, and transparent complication rates are useful indicators when evaluating expertise.
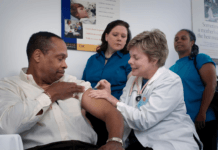
Diagnosis and Tests: What to Expect at Your First Visit
At the initial visit, the specialist gathers a focused history and performs a physical exam, often standing to assess vein appearance and symmetry. The aim is to determine whether symptoms reflect superficial venous reflux, deep venous disease, or another cause such as arterial insufficiency or neuropathy.
Tests and Imaging Used to Evaluate Vein Disease
Duplex ultrasound is the standard test. It combines real-time imaging with Doppler flow studies to identify valve failure, measure reflux duration, and map incompetent veins. Additional tests, such as ankle-brachial index (ABI) for arterial disease or venography in complex cases, are used selectively.
How Specialists Assess Symptoms and Treatment Eligibility
Assessment factors include symptom severity, cosmetic concerns, presence of skin changes or ulceration, and overall medical history (blood clot history, anticoagulation, pregnancy plans). Specialists also evaluate mobility and work demands to align treatment timing with patients’ schedules. Not every visible vein requires intervention: candidacy hinges on functional impact, objective reflux on ultrasound, and realistic expectations.
Treatment Options: From Conservative Care to Minimally Invasive Procedures
Sclerotherapy and Foam Sclerotherapy
Sclerotherapy injects a solution into superficial veins, causing them to collapse and be reabsorbed. Foam sclerotherapy, useful for larger veins, mixes sclerosant with air or gas to increase surface contact. These treatments are office-based, typically require little downtime, and are effective for spider veins and small-to-medium varicosities.
Endovenous Ablation Techniques (RFA, EVLA) and VenaSeal
Endovenous thermal ablation, radiofrequency ablation (RFA), and endovenous laser ablation (EVLA), use heat to close refluxing truncal veins (great or small saphenous veins). They’re performed under local anesthesia with ultrasound guidance and offer rapid recovery and durable results.
VenaSeal is a non-thermal alternative that uses a medical adhesive to close the vein, often requiring less compression afterward. Choice of technique depends on anatomy, prior treatments, and patient preference.
Preparing for Your Appointment and Navigating Insurance Coverage
Preparation reduces anxiety and speeds decision-making. Patients should compile a brief symptom timeline, a list of prior treatments, a current medication list (including anticoagulants), and questions about time off work or travel restrictions.
What to Bring and Questions to Ask Your Specialist
Bring:
- A list of symptoms and when they occur
- Photos showing progression, if available
- Previous ultrasound or medical records
- Insurance card and medication list
Ask:
- What’s causing my veins and what tests are needed?
- Which treatments do you recommend and why?
- What are the risks, recovery time, and expected outcomes?
- How many procedures like this do you perform annually?
- Are staged or combined treatments likely?
Insurance, Prior Authorizations, and Cost Considerations
Insurance often covers treatment when there’s documented venous reflux and symptoms such as pain, swelling, or skin changes. Cosmetic-only procedures may be out-of-pocket. Many clinics provide a benefits check and handle prior authorization. For business owners and remote workers, planning procedures around travel or campaign deadlines avoids disruption. Transparent pricing and financing options are increasingly common. Ask for an itemized estimate before scheduling.
Choosing the Right Specialist or Vein Clinic
Selecting a specialist parallels choosing an agency or vendor: credentials matter, but so do track record, communication, and systems for predictable outcomes.
Key Credentials, Experience, and Clinic Capabilities to Look For
Look for board certification (vascular surgery, interventional radiology, or recognized phlebology credentials), documented experience with the specific procedures being considered, onsite duplex ultrasound, and clear outcome reporting. A multidisciplinary clinic with vascular nursing support and follow-up systems signals higher-quality care.
Questions to Ask to Compare Providers and Treatment Plans
- How many similar procedures has the clinician performed?
- Can they show before-and-after results and patient testimonials?
- What’s the clinic’s protocol for complications and follow-up?
- How will treatment be coordinated with other medical conditions or medications?
For professionals accustomed to vendor selection, request a short discovery call, review case studies, and compare total cost and recovery timelines. Transparent clinics welcome such scrutiny: it’s a sign of reputable practice.
Risks, Recovery, and Follow-Up Care after Vein Treatment
Most modern vein procedures are low-risk, but understanding recovery and potential complications helps set realistic expectations.
Typical Recovery Timelines, Aftercare, and When to Seek Help
Recovery depends on the procedure type. Sclerotherapy often allows return to normal activity the same day, while ablation may require a few days of limited high-impact activity and wearing compression stockings for 1–2 weeks. Ambulatory phlebectomy might cause minor bruising and a short period of soreness.
Follow-up typically includes a clinic visit and a repeat duplex ultrasound within weeks to months to confirm vein closure. Patients should seek immediate care for signs of infection, increasing pain, significant swelling, or symptoms of deep vein thrombosis (sudden calf pain, pronounced swelling, chest pain, or shortness of breath).
Possible Complications and How Specialists Minimize Risk
Complications are uncommon but can include skin staining, matting (new small vessels), transient nerve irritation, superficial thrombophlebitis, or, rarely, DVT. Specialists minimize risk with careful pre-procedure assessment, ultrasound guidance, sterile technique, and clear post-procedure instructions.
High-volume centers with structured follow-up tend to detect and manage issues early, reducing long-term sequelae.
Conclusion
A qualified varicose vein specialist turns a common complaint into a manageable condition with durable, low-risk solutions. For professionals balancing packed schedules and outcomes-driven decisions, choosing a clinic with strong credentials, transparent outcomes, and efficient logistics preserves both time and health. Whether the goal is symptom relief, prevention of complications, or cosmetic improvement, an evidence-based, minimally invasive approach usually provides the best combination of safety and effectiveness. When in doubt, an evaluation and duplex ultrasound is a small time investment that can prevent bigger problems later, and get someone back to work, travel, and life with greater comfort and confidence.